Dr. Donald Lysle is an expert in neural immune signaling and opioid effects on the immune system. An exciting new intersection of these two fields of expertise has culminated in his recent work with an animal model of Post-Traumatic Stress Disorder (PTSD).
PTSD is a common psychiatric disorder that results from exposure to a severe threat to psychological or physical bodily integrity. It is characterized by chronic anxiety and exaggerated fear learning that is resistant to extinction. The military deployed about 2.5 million troops to Iraq and Afghanistan, approximately 13%-20% of which are estimated to have developed PTSD [1]. Unfortunately, there are currently no effective pharmacological treatments for PTSD and the ones in current use have small effects with unclear clinical relevance [2]. Clinical correlational studies have found that morphine treatment in the hours after a combat injury is associated with a significant reduction in PTSD rates among combat veterans [3, 4]. A similar correlation was found in children who experienced a single-incident trauma that required an emergency room visit [5]. Investigations in our laboratory are aimed at understanding the neurobiological underpinnings of PTSD.
 Dr. Lysle and his research team established the first animal research that supports the use of morphine as a prophylactic pharmaceutical treatment for PTSD [6]. In these studies, rats were exposed to the stress-enhanced fear learning (SEFL) paradigm, an animal model of the disorder [7], and administered morphine at different times following the initial traumatic stress. The results showed that morphine completely blocks the development of SEFL when administered 48 hours, but not immediately, following the initial trauma [6]. Importantly, any analgesic effect of morphine would be most potent if administered immediately after the trauma, thus, in our experimental model, morphine appears to have a preventive effect on the development of SEFL beyond its analgesic effect following trauma. Current studies are aimed at exploring glial cell function and neural immune signaling as a mechanism through which morphine exerts its effects on SEFL. We recently published the finding that severe stress induces a time-dependent increase in IL-1β within the dorsal hippocampus that was causally related to the development of SEFL and that morphine administration attenuated this increase [8].
Dr. Lysle and his research team established the first animal research that supports the use of morphine as a prophylactic pharmaceutical treatment for PTSD [6]. In these studies, rats were exposed to the stress-enhanced fear learning (SEFL) paradigm, an animal model of the disorder [7], and administered morphine at different times following the initial traumatic stress. The results showed that morphine completely blocks the development of SEFL when administered 48 hours, but not immediately, following the initial trauma [6]. Importantly, any analgesic effect of morphine would be most potent if administered immediately after the trauma, thus, in our experimental model, morphine appears to have a preventive effect on the development of SEFL beyond its analgesic effect following trauma. Current studies are aimed at exploring glial cell function and neural immune signaling as a mechanism through which morphine exerts its effects on SEFL. We recently published the finding that severe stress induces a time-dependent increase in IL-1β within the dorsal hippocampus that was causally related to the development of SEFL and that morphine administration attenuated this increase [8].
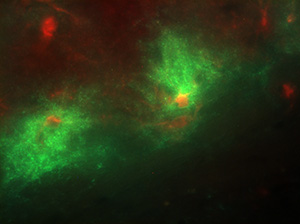
Our most recent work has taken advantage of cutting edge chemogenetic technology. Dr. Lysle and Meghan Jones, doctoral fellow in Behavioral Neuroscience, have employed glial-expressing Designer Receptors Exclusively Activated by Designer Drugs (DREADDs) to examine the role of hippocampal astrocytes in SEFL [see photo]. DREADDs are synthetically engineered muscarinic receptors that have lost their affinity to acetylcholine[9]. Viruses are used to site-specifically create receptors in the brain that can be activated by Clozapine-n-Oxide (CNO), an otherwise pharmacologically inert ligand that will cross the blood brain barrier when injected peripherally and activate GPCR signaling in cells expressing the receptor. With these receptors, Dr. Lysle can infuse CNO peripherally to activate either Gq or Gi signaling specifically in hippocampal astrocytes.
 We are excited about the preliminary studies using this technology that are currently underway. Collectively, our research in the Lysle Lab aims to elucidate the neurobiological underpinnings of PTSD and ultimately identify targets for the development of prophylactic pharmaceutical treatments for the disorder, with less abuse potential than morphine. Dr. Donald Lysle is a Kenan Distinguished Professor and Chair of the Department of Psychology and Neuroscience.
We are excited about the preliminary studies using this technology that are currently underway. Collectively, our research in the Lysle Lab aims to elucidate the neurobiological underpinnings of PTSD and ultimately identify targets for the development of prophylactic pharmaceutical treatments for the disorder, with less abuse potential than morphine. Dr. Donald Lysle is a Kenan Distinguished Professor and Chair of the Department of Psychology and Neuroscience.
1. Hoge, C.W., et al., Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med, 2004. 351(1): p. 13-22.
2. Hoskins, M., et al., Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry, 2015. 206(2): p. 93-100.
3. Holbrook, T.L., et al., Morphine use after combat injury in Iraq and post-traumatic stress disorder. N Engl J Med, 2010. 362(2): p. 110-7.
4. Melcer, T., et al., Glasgow Coma Scores, early opioids, and posttraumatic stress disorder among combat amputees. J Trauma Stress, 2014. 27(2): p. 152-9.
5. Nixon, R.D., et al., Predictors of posttraumatic stress in children following injury: The influence of appraisals, heart rate, and morphine use. Behav Res Ther, 2010. 48(8): p. 810-5.
6. Szczytkowski-Thomson, J.L., C.L. Lebonville, and D.T. Lysle, Morphine prevents the development of stress-enhanced fear learning. Pharmacol Biochem Behav, 2013. 103(3): p. 672-7.
7. Rau, V., J.P. DeCola, and M.S. Fanselow, Stress-induced enhancement of fear learning: an animal model of posttraumatic stress disorder. Neurosci Biobehav Rev, 2005. 29(8): p. 1207-23.
8. Jones, M.E., et al., The Role Of Brain Interleukin-1 In Stress-Enhanced Fear Learning. Neuropsychopharmacology, 2014.
9. Zhu, H. and B.L. Roth, DREADD: a chemogenetic GPCR signaling platform. Int J Neuropsychopharmacol, 2014. 18(1).